Infertility, IVF, Miscarriage, High Risk Pregnancy, and Rainbow Birth Story
The Frozen Embryo Transfer
October 27, 2021 was our 4th embryo transfer.Our 3rd transfer had brought us our daughter, Tayvri. I prayed that by doing the same FET (frozen embryo transfer) protocol, we would become pregnant the first try this time. Yet, I was still anxious of the what if's, and weary of the potential pain coming our way.We decided to transfer 2 embryos, knowing it had taken 3 transfers with 5 embryos to get our rainbow daughter Tayvri. Also, our embryos were untested so we hoped putting 2 in would increase our chances of success.
For the few who knew we were going in, we lied and said we were transferring only one.
With IVF, so much of the surprise gets taken away and IF we got pregnant with twins, we wanted so badly to surprise everyone.
Well, we got pregnant!
I suffered from severe morning sickness and was trying to hide it from almost everyone. None of my co-workers knew as I would sneak saltines in my mouth, or slip away to administer my progesterone shots. I was giddy with excitement thinking about the day I would surprise them all!
At Thanksgiving dinner, I pulled my grandmother aside and told her about the twins. She was the first person to know and we hugged as we cried. She said it was such a blessing and that she and my grandfather had been praying for us.
After Thanksgiving, when just my immediate family was together, we put a picture of us holding the ultrasound photo on the big screen. Tears of happiness streamed down my face as my family screamed remarks of joy!
I purchased twin dolls, two doll cribs, and a double doll stroller to be opened by Tayvri on Christmas morning with my husbands family. We planned to use it as an announcement to them about the twins. I knew they would be extra excited because they have a set of twins in their family.
They looked at the second baby.
Again, no movement, no heartbeat.
I could feel the hot tears swell in my eyes as I laid there in that too quiet room. My husband squeezing my hand as the ultrasound tech said, "I'm sorry".I have been through some devastating things in my life. Many of which I have written elsewhere on this blog. But I think in that moment, and in the days following, I felt this was the most painful thing I had experienced.
I was mad at myself. How could I have let my guard down so quickly? Foolish. Why did I not think this would happen? Why was my body not a safe place for these babies to grow?
I went for a repeat ultrasound the next day which verified the miscarriage. I then underwent a D&E the following day. I remember going to bed the night before realizing this was the last couple of hours with my twins inside me. A sense of wanting to be done with the tragic experience replaced with not wanting to let them go.
The next morning, I remember laying on that cold operating table, still nauseous from the pregnancy, and saying my 'goodbyes for now' to my sweet babies as they put that mask on my face and I drifted off to sleep.
We sent the twins remains to be genetically tested, looking for answers to the loss. What we learned was that I had been carrying two genetically perfect babies. And they were girls.
I think learning the genders gave me some closure as it helped us to name them. However, learning there was nothing wrong with them was difficult because then I knew it was my body which had failed them.
While we were waiting for the genetic results, we decided to also take our remaining 6 frozen embryos and have PGT (preimplantation genetic testing) done. We didn't originally do PGT on our embryos because we had 13 from our retrieval (this is a lot), and it was VERY expensive to test that many. I was 28 when we retrieved them and my age gave a higher chance of the embryo's being good quality. There is also mixed opinions on the value of PGT results and the likelihood of successful live births. But I did not want another loss and was willing to do anything.
It cost an extra $3,470 to have these 6 embryos thawed, genetic testing done, and then re-frozen.
What we learned was we had 5 genetically perfect babies. And we have 1 "mosaic abnormal" with a +19, +20, +22. This leaves little chance at life for that embryo. However, we have chosen to keep them on ice for the present time. (If you are reading this and have any experience with this type of complex abnormal embryo, please reach out to me).
While we were very happy to have such incredible results, and my RE's (reproductive endocrinologist, i.e. our fertility doctor) office said it is uncommon to see such high percentages of normal embryos, it did not give us answers to why we kept miscarrying. So we ran more blood work. My vitamin D was low so I began supplementation. Then we found I was compound heterozygous MTHFR (with no other clotting factors). In short, this means my body can't absorb folic acid and needs the naturally occurring form of methylfolate. So I began a new-and expensive-prenatal vitamin regimen, along with some diet changes.
Christmas 2021 was supremely difficult.
News travelled around about the loss of our twins. I hated the pitiful looks, the sympathetic hugs, the well meaning words of hope. I knew everyone had our best interest, but it just hurt.
January 2022 came and we began preparations for our next FET. I went in for my required water ultrasound and my lining didn't look right. So they scheduled me for a hysteroscopy.
During the hysteroscopy they found 14 polyps had grown in my uterus! My RE was amazed, as he had just "cleaned" out my uterus in the D&E. He removed the polyps and told me as long as they could get my lining to thicken back up, I would be cleared for my next FET in February.
However, February came and my transfer had to be cancelled due to fluid in my uterus. It felt like road block after road block! They put me on some antihistamines to help dry it up and moved my transfer to March.
March came and everything finally looked perfect. We decided to transfer 1 embryo this time. We asked our RE to transfer the next best embryo and keep the gender a secret.With each transfer comes a month of shots, medications, ultrasounds, blood work, and immense preparation. The anticipation is killer! There is a lot of excitement, hope, fear, and faith involved. Then transfer day comes and is followed by the longest most grueling 10 days of your life, affectionately called the TWW (two week wait). This is the wait for your blood beta HCG test to confirm if the transfer was successful and you're pregnant or not.
 |
| Upgraded my lucky transfer socks |
 |
| White spot in the middle is the embryo |
 |
| IYKYK |
Day 5: negative.
Day 6: negative.
Day 6 in the evening: very faint line.
I felt a glimmer of hope! Maybe this embryo is a late implanter? I searched the internet for success stories and found many which fueled my hope.
Day 7: still a very faint line. But I knew it takes 2 days to double and so one really should look at every other day line progression.
However, day 8 came and the line still looked the same. Despair filled my mind again. Not another loss, I prayed.. I couldn't handle it.
Day 9, maybe the line is darker? I couldn't tell. I spent the day going in the bathroom every hour to hold the tests in different lighting trying to determine how dark the lines were.
On the morning of day 10, I finally had enough HCG in my system to show positive on a digital test! I felt so much hope again as I drove in for my beta HCG.
Afterwards I sat with my phone, checking it every couple of minutes, waiting anxiously for results.
The results came.
15.
I knew this was not good. Ideally my clinic wants it to be above 100, and preferably over 200 at this point. I spent the rest of the day crying.
My RE sent me for a repeat test two days later. We were looking for at least a 60% rise. However, my results were only 26.In the infertility world, they call this Beta Hell. This is when your HCG is not rising appropriately and you have to continue going in for repeat blood work until they either confirm you are miscarrying, or they feel satisfied that things are progressing well.
Two more agonizing days passed excruciatingly slow, while I wrestled in my mind between hope and discouragement. When the results of my third beta finally came in, it confirmed we were miscarrying. My HCG dropped to 17. They call this a chemical pregnancy, meaning a miscarriage before 5 weeks of gestation. This was going to be our sixth angel baby.
I text my clinic nurse because I needed to know. What was the gender of this sweet baby I was losing? She responded, it was a Boy.It felt so unfair. Why was my body not carrying these perfect babies?
I turned to Heavenly Father as I needed a renewal of understanding concerning the welfare of their souls. As I pondered and searched for an answer, it came to me some months later while driving my car: my babies are in Heaven. They are not lost. They were not nothing. They are being cared for by mine and Trevor's ancestors, and we will see them again.
My RE, Dr. Foulk, asked that we make the 3.5 hour trip to his main office to see him in person. He wanted to do an exam himself. (There is a main office with multiple smaller offices scattered around. He is only in the St. George office a couple times a year. When he isn't there, I speak with him remotely and I see a Nurse Practitioner and other staff in the local office).
He came in and did a thorough ultrasound, during which he confirmed his suspicions that I had developed Adenomyosis. This is a condition where the endometrial tissue grows into the uterine wall. It is similar to endometriosis, which I also have, but with endometriosis the endometrial tissue grows outside of the uterus and into other parts of your body. He explained adenomyosis like this: typically your uterine wall should be a beautiful field of soft soil, ready to be planted. But with adenomyosis, the soil is filled with rocks.
 |
| See my saved stories on IVF #6 for details about the above photo |
He then told me something very interesting, he said he used to diagnose adenomyosis 1-2 times per year, but since the C*vid Va**ine, he now diagnoses it 1-2 times per week. That is a different discussion for another time though.

He suggested we complete a 3 month round of Lupron Depot. I was familiar with this drug because I had used it for my stage IV endometriosis back in 2015. It is a hormone suppression drug used to calm the endometrial tissue. The purpose would be to improve my uterine lining, trying to make it a lush soil again for an embryo to attach and grow.
Unfortunately, the drug is very expensive and has awful side effects. These effects include mood swings, weight gain, acne, hot flashes, bone pain, etc... I knew I had survived before and I was determined to survive it again!
 So in May 2022, I went to the fertility clinic and received the first Lupron Depot shot (I did the rest myself at home). Then in July, we did a repeat HSG (hysterosalpingogram) to make sure I did not have hydrosalpinx in my tubes. (This is where fluid collects in your fallopian tubes and that fluid can spill out and cause miscarriage). I had the procedure done before back around 2013, and it was quite painful the first time. Thankfully, the HSG went smoothly and it wasn't painful this time.
So in May 2022, I went to the fertility clinic and received the first Lupron Depot shot (I did the rest myself at home). Then in July, we did a repeat HSG (hysterosalpingogram) to make sure I did not have hydrosalpinx in my tubes. (This is where fluid collects in your fallopian tubes and that fluid can spill out and cause miscarriage). I had the procedure done before back around 2013, and it was quite painful the first time. Thankfully, the HSG went smoothly and it wasn't painful this time. I couldn't believe we were coming up on a year of trying to conceive again. I felt exhausted by all the road blocks. 2 new miscarriages, 3 surgeries, multiple new diagnoses and medications, so much money and time. I questioned if all the efforts were taking too much time away from Tayvri. It felt selfish to be trying so hard for a second child when I already had a beautiful and perfect daughter who deserved all of my attentions.
I was studying the Old Testament during this time. And just prior to our 6th transfer, I was reading 2 Kings 4:16 which says:
"...About this season, according to the time of life, thou shalt embrace a son..."
In that moment, I knew Heavenly Father was speaking to me. The Spirit testified to me that I would have a living child in my arms by that time next year. I didn't know if it would be a son, but I KNEW a baby was coming. Peace filled my heart that the time and efforts put into trying for this second child were worthy and the blessing was coming.
 |
| Nivestym to make my uterus "sticky"! |
Finally in August 2022, we were cleared for another FET. This would be our 6th embryo transfer. We again asked our RE to put in our single next best embryo and to keep the gender a secret from us.
Besides the completion of 3 months of Lupron, the repeat HSG, and the hysteroscopy, Dr. Foulk also agreed to daily lovenox injections for this next round. He called it the "kitchen sink method", where we threw everything we could into the mix to increase our chances.
Also, some studies show increased success rates for patients with MTHFR using anticoagulants in pregnancy. I took the lovenox in conjunction with baby aspirin.
This time, we drove the 3.5 hours to the main office for implantation day. August 25, 2022. I was a ball of nerves! Although I felt confident a baby was coming, I didn't know if it would be from this transfer, or in some other way.
The transfer went perfect. It is always such a strange experience walking into the clinic knowing you aren't pregnant, only to walk out 30 minutes later knowing you are carrying a living embryo inside of you. In the infertile world we call this PUPO: pregnant until proven otherwise. Then all you can do is pray that embryo attaches to the uterine lining and continues to live.
 |
| New lucky transfer socks since my others didn't work! |
 |
| IYKYK |
We got some McDonalds fries, and then drove the 3.5 hours back home. I then took my 3 day valium nap. (My RE prescribes me valium 10mg every 8 hours for 3 days to prevent uterine cramping due to my history. I lovingly call this my 3 day nap, which admittedly, I thoroughly enjoy!) *You can read more about my transfer protocols on my first IVF blog post.*
The Pregnancy
On the fourth day, I snuck out of my bed in the early morning, per my usual, and peed on a stick.
The faintest little pink line stared up at me.
I've always wanted to do some cute way of telling my husband we're pregnant. Yet, every time I find myself immediately running and jumping in bed, startling him awake and wildly yelling "we're pregnant!"
Day 5, the line was definitely darker. Good news!
Day 6, the line was the same as the day before.
Day 7, the line looked fainter.
It was Labor Day weekend, so my clinic was drawing my beta HCG on day 8 since they would be closed for the long weekend.
I was so afraid going in for my blood draw. I told the phlebotomist that I knew I was pregnant, but I was pretty sure we were losing the baby.
I collapsed to my knees in my closet saying out loud, "I can't do this".
That's when for the second time in my life, I physically felt arms around me. Multiple arms from unseen angels, there to support me. And the words in my ear saying "all is well".
Peace filled me and I knew I had the strength to carry on through another round of Beta Hell.
I had to wait 4 days, through the long weekend, for my repeat beta. We had plans to go to my husbands family cabin that weekend, but I was a wreck and we cancelled last minute.
I peed on SO many sticks but saw little to no line progression.
My husband offered me a priesthood blessing and in it he stated, "all is well".
I had not told him about my experience, yet somehow he used that EXACT wording.
By the time I went for my blood draw Tuesday morning, I was mentally prepared for bad news. In my head I had accepted this as a chemical pregnancy and was making plans for our next steps.
When the nurse called, I could not believe my ears as she exclaimed, "263"! I needed her to repeat it because I was sure I heard wrong. Again I fell to the ground in tears, but this time it was tears of joy!
Since we were looking for a 60% increase, we would have been happy with anything over 110. 263 was a 160% increase! I remember my shaky fingers as I called Trevor. We were both overwhelmed!
We knew that good doubling times didn't equal a continued pregnancy, with our twin girls our doubling time was beautiful but we still lost them.
And with our daughter, the doubling time was barely 60%.
We allowed ourselves to be cautiously excited about the pregnancy and celebrated with ice cream.
The next morning I woke up to blood in my underwear.
I called the clinic. I was scared.
Usually my clinic does your first ultrasound at 7 weeks. However they agreed to get me in right away due to my extensive history and the bleeding. So at 5 weeks and 4 days pregnant, we went in for the first ultrasound.
I was apprehensive and held my breathe as they placed the ultrasound probe.. Peering up at the big screen, there it was. A perfect tiny speck of a baby on the screen. We could see a sac and a fetal pole. There was a small SCH (sub chorionic hemorrhage) which must have been the cause of my bleeding.
Then the clinic surprised me as they explained I was actually 5 weeks and 6 days pregnant! I had not realized when they thawed my embryos for genetic testing that they had aged.
So instead of implanting a 5 day old embryo, they had implanted a 7 day old embryo.
I was elated by this news. You see in early pregnancy after loss, each and every day feels like a milestone. It was good to know I was that much closer to 6 weeks pregnant. Then on to making it through the first trimester and then to 40 weeks!
At our 7 week ultrasound we listened to the baby's heartbeat. Such a beautiful moment! Crazy knowing that sometime within the prior week this little heartbeat suddenly started within me, how magical!
The baby measured perfectly but the sac around the baby was surprisingly small, measuring 7 days behind..
Concerned, I turned to google. I found few studies on small sac's, termed "small gestational sac syndrome". I called and spoke to the Nurse Practitioner at the clinic, who apparently was also doing research on it. She told me there was 60-80% chance of miscarriage before 10 weeks with this diagnosis. The studies had no guidance on anything to do to help the situation. So she recommended weekly ultrasounds to keep an eye on things. She also suggested I try my best to preserve water in my body via drinking LOT's of water, low salt diet, no caffeine or other diuretics, and no sweating. Our goal would be to make it past 10 weeks.
As you can imagine, this was devastating news to us. I lived each day pleading with God to save this baby.
The weeks passed tormentingly slow. When people asked how I was doing, I would nod because words only brought tears. I didn't want anyone to know how afraid I was. How do you explain the pain you are going through to someone else? Living with the fact that your baby could literally be dying inside your body at any moment without you knowing. No one could understand except my husband and my Savior.
Our ultrasounds went like this:
I would hold my breath as they inserted the probe until I could see if the baby was alive. Then they would measure things and I would go home to stress about it for another week.
At 8 weeks 1 day, the sac was 9 days behind.
At 9 weeks 1 day, the sac was 13 days behind.
At 10 weeks, the sac was 14 days behind.
It wasn't until our 12 week ultrasound, with the sac still 15 days behind, that I began feeling like I could breathe again.
The baby was growing right on track, kicking and wiggling around, seemingly unperturbed by the squishy space.
*Some studies suggest that small gestational sac syndrome may be more common than presently known. This is because many pregnant women are not getting ultrasounds prior to 12 weeks and after 12 weeks the sacs are not measured. *
**I have had a handful of women reach out to me after receiving this diagnosis and finding me online, some have had happy outcomes and sadly some have not.**
We graduated from the fertility clinic after that 12 week appointment. I will be forever grateful to them for not only getting us pregnant, but holding my hand through those weeks of unknown.
It was nerve-wracking going from weekly ultrasounds to the normal OB appointment schedule. But I tried to trust God's promise to me and the doctors that were telling me the baby was growing well!
Thanksgiving came, I was 16 weeks and beginning to settle into the pregnancy, feeling more confident and excited.
The day after Thanksgiving, I had a strange sensation of urinary hesitancy. I dismissed it until that Saturday night when I woke up to pee and couldn't get anything out! Worried I might have a UTI, I chugged some water before falling back to sleep. I woke a couple hours later urgently needing to urinate, but again nothing came out! I was now very concerned that something else was going on.
I sat on the toilet for over an hour, trying all the techniques that, as a nurse myself, I tell my own patients to help them urinate. Nothing was working. I was beginning to be in a lot of pain. It had been at least 9 hours at that point since I had peed, I knew my bladder was full, and I desperately needed to go!
So I finally called my OB's after hours line. I already knew what they would say, but pridefully I hoped I was wrong.
"Go to the Emergency Room".
Having previously worked in an Emergency Room, I knew the protocol for urinary retention. And it didn't sound fun to me! I knew it needed to be done though. I needed a foley catheter. And at that point my pain was beginning to be unbearable.
We checked in, and I am serious when I say that by the time I was in that ER room, I felt my pain was worse than my previous unmedicated birth! This is because it was constant, unlike contractions.
My belly appeared to have grown twice the size. My blood pressure was elevated (it didn't even elevate with my unmedicated delivery). I paced the room.
Luckily, I knew some of the staff working, including the Physician Assistant assigned my case. They worked quickly and inserted a catheter which drained 1,300mL's of urine.
I felt AMAZING after. So much relief!
They did an ultrasound and found our cute 16 week baby wiggling around, thankfully undisturbed from the fiasco.
They were unable to determine the cause of the retention. There was no UTI and no other concerning symptoms, so they sent me home to follow-up with urology 2 days later. Unfortunately I had to keep the catheter in, when the bladder stretches that much it can lead to further urinary retention if not given the chance to recuperate.
I did some research and was pretty sure I knew the culprit. My Midwife had diagnosed me with anterior cervical wall prolapse at my last appointment. I figured the prolapse had become bad enough that it was blocking my urethra. I called my Midwife and requested an appointment before the Urologist to confirm my suspicions.
So Monday morning I toted myself, catheter and all, in to see the Midwife.
Upon exam, she found I had a rare condition called an "incarcerated uterus" or "trapped uterus". It wasn't the prolapse causing the problem, it was my uterus. It was tilted so far backwards that it was trapped in my pelvic cavity, stuck between my pubic bone and my spine. It was pressing on my urethra and blocking my ability to urinate.
The Midwife had heard of this but had never seen it. She explained the first-line treatment is manually pushing the uterus up into place. She did not feel comfortable preforming this herself, so she called the OB to come.
The OB told me he had only seen an incarcerated uterus a couple times in his career but he felt confident in his ability to manually fix it.
They had me lay back on the exam table. It only lasted a moment, but my goodness it was incredibly painful! A lot of pressure... Afterwards, he stated it only moved a small amount but he could not get it to "pop" into place. His recommendation was to wait and see what happened over the next 4 weeks. If the uterus didn't pop up by 20 weeks, then I would go under anesthesia to have it corrected.
Tuesday morning I met with the Urologist. He agreed to have the catheter removed so we could see if the OB had moved the uterus enough to resolve the urinary retention. Thankfully, I was able to pee on my own within a couple hours!
At my appointment the following week, the Midwife confirmed my uterus had indeed popped up. (Though they did tell me that I am likely to experience an incarcerated uterus in future pregnancies).
I couldn't believe the curve balls this pregnancy kept throwing me. And to top it off, I was still so nauseated and having serious food aversions! Little did I know, the nausea wouldn't let up until 28 weeks, and the curve balls were far from over.
 |
| Bruising from Lovenox |
My Midwife thought it might be good for me to see MFM (Maternal Fetal Medicine, a.k.a. the high risk pregnancy doctor) for my anatomy scan. This was mostly because she wanted a second opinion on my MTHFR and Lovenox management around birth.
So at 22 weeks, we finally went for the scan. I remember being very excited to see the baby. My husband took work off to be there and we got a babysitter for our daughter.
I am a member of a Facebook mom group for IVF babies that were due at the same time. I had seen a post recently about incorrect cord insertions, so it was fresh on my brain. I remember as the ultrasound tech looked at the cord, it appeared to be center in the placenta and I commented how that was a good thing and the tech agreed.Apparently the MFM Doctor I was seeing liked to do a scan check herself, so when the tech was done, they left everything set up for the MFM. She came in and as she scanned, we chatted about my plan for another unmedicated birth. She was excited for me and talked over a plan for the blood thinners around delivery. However, she then became quiet as she saw something on the screen.
She turned to us and said I had a Valementous Cord Insertion (VCI). This meant that the baby's umbilical cord was inserted in the membranes of the sac instead of the center of the placenta as it should be. Weird, I thought, as it didn't look that way when the ultrasound tech went over it. Immediately I was grateful that the MFM was so thorough!
She explained that most of the time VCI does not cause problems, but in some cases, it can lead to growth restriction of the baby. So they would plan to do repeat growth ultrasounds in my third trimester. She also explained that it could interfere with my unmedicated delivery. She recommended closer monitoring of the baby's heart rate during labor due to the exposed cord vessels, which could compress easier leading to heart decelerations. In some cases this could lead to the need of a cesarean section, so it was worth discussing possibly having an epidural in place.
I really did not want to hear these things. My heart was completely set on an unmedicated delivery. I absolutely loved my hypnobirth with my daughter and I was immensely looking forward to doing it again. It was the first thing I was excited about when we had become pregnant, and I was already preparing for it.
She told us because of the VCI, she had to do a vaginal ultrasound as well to rule out Vasa Previa (VP), which was very rare, but could occur with VCI. She left the room so that I could undress from the waist down.
I had never heard of VP, but it sounded intense. So I remember praying with Trevor for comfort and a level head about whatever the diagnosis would be. The Spirit was there with us, and we both felt peace about the situation as we waited for the Doctor to come back.
The vaginal ultrasound confirmed I did had VP.
The MFM's tone became serious as she explained this was an extremely rare condition. It was often fatal to newborns if not diagnosed prior to delivery. She told me it was a very good thing I was there that day and that it had been found. With proper diagnosis, VP babies have a very high chance of live birth. However, for safety I would need to have a cesarean section between 34-36 weeks gestation.
**About 1 in 200 pregnancies will be diagnosed with Placenta Previa, while only 1 in 2,500-5,000 pregnancies will be diagnosed with VP, though it is more common with IVF pregnancies. This means a woman is 10x more likely to naturally conceive twins than to have VP.**
My head was spinning as she explained the condition. Basically the baby's umbilical cord was attached to the membranes (think the bag of water the baby sits in). From there, fetal blood vessels come out from the attached spot and travel to the placenta. This is the VCI. However with VP, the vessels run directly over, or within close proximity to the cervical opening. This is dangerous because as your cervix begins to dilate, or if your water breaks, the baby's blood vessels can easily burst open and the baby can bleed out within a matter of minutes.
She went on to tell us that in addition to a preterm c-section delivery, we should not travel more than 15 minutes from the hospital after 24 weeks pregnant. I was told no heavy lifting, no squatting, no inserting anything into the vaginal canal, and absolutely no cervical checks. I was to immediately go to Labor and Delivery if I had any spotting or bleeding.
I went home and immediately turned to Google to learn everything I could. I saw a lot of scary things on there. I don't recommend it!
I then found a Facebook support group where I read many positive stories. The women on there called their VP babies Survivors. Survivors.. what a powerful word. But I realized it was true.
During my research, I found the general VP protocol was to admit the pregnant woman around 30-34 weeks gestation to await delivery. This ensured that should any bleeding begin, they were within minutes to an Operating Room for an emergency delivery. The further the pregnancy progresses, the higher likelihood of bleeding due to the growing baby, or the cervix starting to dilate. Also, women with VP have a higher chance of preterm labor.
However, MFM hadn't mentioned anything to me about being admitted antepartum? My next appointment was not until 28 weeks, 6 weeks away, which felt like a lifetime.
That night I went to a group reading with a Medium named Ang. This was not my typical event to attend, but I had a good friend invite me and I was curious. After the event, Ang told me that my baby was golden and she guessed the birthdate to be a month early. This was without me telling her anything about the pregnancy or the need for an early c-section. She told me this baby was coming, there was nothing that could stop it, it would have a name and a heartbeat and come home with me. Ang later told me the baby would be a girl and that she would bring a lot of healing into my life. Ang gave me a guarantee, which she says has only happened three times in her career.
*I was selected for a palm reading on a podcast, you can listen to it and hear what Ang says about the baby on Spotify: Get Soul Inspired.*
We had purposely not learned the gender and planned to wait for delivery to find out. I however, was completely convinced this baby was a boy! In fact, I was so convinced it was a boy, that I told my husband we didn't need to wait to find out because it wasn't going to surprise me anyways! So I wasn't sure what all I believed from my palm reading, but I loved the comfort I received from it during such an emotional time.
During those 6 weeks, my OB office had me swap from the Midwife to the Doctor for my care.
When I asked if he had taken care of someone with VP, his answer was, "once every 10-20 years". I could have been nervous, but it seemed he was doing a lot of research along side me and his plan was to follow MFM's guidance.I went through a grieving period for the birth I had envisioned. A c-section was not what I wanted. I had required all sorts of interventions to get pregnant (both times) and my previous natural delivery had been so healing for my soul. Through it, I had proved to myself that my body was capable after nearly a decade of believing it was broken. I had never felt so strong or so powerful then I had during my hypnobirth.
I was devastated about a c-section.
But at the same time, I was grateful knowing c-sections are commonly preformed and generally safe. I used to work as a scrub tech for c-sections in a L&D back in 2015, so I was very familiar with the process. I started to envision my delivery in a new way, meeting my baby, not by catching them as they came through the birth canal, but peering up at them over the sheet as the doctor pulled them up and out of me.
I spent those 6 weeks in a mix of fear and faith, fretful of an emergent delivery, but continually hearing in my mind, "all is well". I felt so robbed of the whole pregnancy experience.
At 28 weeks we finally went back for our next MFM check-up. The first MFM we had seen wasn't there that day and we saw a different one. He and the ultrasound tech thoroughly examined the baby and the cord. I remember them humming and ahhing at each other. I finally spoke up to ask what was wrong. He was excited as he told me that my VP had resolved, the vessels had grown up and away from the cervix and I could now have a vaginal delivery. I was shocked.
He could tell I was in disbelief, so they tilted the table backwards and pushed the baby's head up so they could see the cervix, but still no vessels were seen. Despite my apprehension, he assured me I didn't need to come back for a growth scan until 34 weeks.
Trevor and I went home, feeling unbalanced over the mixed emotions. Could I have my dream hypnobirth again? Were we going to be able to carry this baby full term? Could I stop fearing every minute of every day about losing our child?
Something didn't feel right. I just knew it in my gut.
I called the next business day, asking to speak to the original MFM who diagnosed me. When that MFM called me back, she agreed we should exercise extreme caution and do a repeat ultrasound at 30 weeks to confirm the resolution.
So at 30 weeks we went back in. I didn't know what to expect. I had this gut feeling, but I didn't want it to be true. The day before, I had prayed to Heavenly Father that a proper diagnosis could be made and that I would trust it. I asked in my prayer for the baby to be breech for the ultrasound because I knew this would make it easier to see the cervix.
The baby had been consistently head down at every appointment since 22 weeks, so when they put the ultrasound probe in and found the baby feet down in breech position, I was surprised and very thankful!The MFM immediately saw the large vessels within 2cm of my cervix. They were still there. I still had VP. Thanks to the baby's head not being in the way, they could now be seen easily. It was a huge relief to me knowing I had listened to the prompting to have this repeat ultrasound. Though I did not want to have VP, I know that if it had been missed, we likely could have lost our baby. This makes me angry at the confidence the other MFM had in telling me it had resolved. It also makes me want to educate others to advocate for their healthcare and trust their mama guts. What a whiplash.
We went back to my original care plan. I started weekly NST's (non-stress tests) and AFI's (amniotic fluid index), with a plan to repeat a growth ultrasound at 34 weeks. At that time they would determine my delivery date. Upon asking about hospitalization, the MFM was hopeful we could manage outpatient but if there were any signs of pre-term labor we would admit me to the hospital.
 I should mention that around this time, I failed my glucose tolerance test and was diagnosed with gestational diabetes. It was the cherry on top of everything. Just when I wanted to eat my feelings away, I was put on a diet. Lucky me!
I should mention that around this time, I failed my glucose tolerance test and was diagnosed with gestational diabetes. It was the cherry on top of everything. Just when I wanted to eat my feelings away, I was put on a diet. Lucky me!
I went in for my 31 week NST/AFI. 
At my next NST, they again saw a contraction, thankfully this time it did not effect the baby. However it prompted the discussion between me and the MFM that it would be safest to have me in the hospital. We planned to admit me at 34 weeks.
I felt torn as I prepared to leave my daughter at home while I went into the hospital to await the arrival of this new baby. I knew the hospital was the safest place to be but how could I leave my daughter during those last couple weeks of her being my only child?
We had a whole plan for the day I would be admitted. Trevor would take the day off work and we would spend it together, our last full day together as a family of 3. We would eat a yummy dinner and then drop me off, somehow finding a way to explain to my daughter that mommy had to stay at the hospital for a while.Life has a funny way of changing your best made plans.
At 33.1 weeks, I went in for my NST. They were beginning to blur together and seem routine. Go in, have a quick AFI, then get hooked up. Listen to the baby's heartbeat for 20-30 minutes while playing on my phone. Sometimes have short discussions with the diabetic educator there. Get unhooked and go back home.
But that day, I had another contraction which resulted in a deceleration of the baby's heart. So they wanted to keep watching. Then the monitor picked up another variable. The nurse came in and said MFM was advising I go upstairs to L&D (Labor and Delivery) for an extended monitoring session. She told me it may last 1-2 hours, or sometimes overnight. She was nice and thought to bring me in a salad and cheese stick to eat quickly before I went up.
I could feel some anxiety creep in but I tried to sound nonchalant about it as I called my husband. I told him not to worry, stay at work and I would update him. Then I called my mom to see if she could pick Tayvri up.
Hospital Stay
It was weird walking into L&D by myself, worrying about the baby and feeling guilty about missing lunch with Tayvri. I didn't realize then that I would not be leaving for three weeks.
They had me change into a gown, collect a urine sample, and get hooked up to the monitor. The room quickly felt lonely as I laid in the bed listening to the baby and wondering what the doctors were thinking.
Trevor called me and said he had decided to come anyways. This made me happy.
I am glad he was there because I began having contractions. They were noticeable but not painful and they were 3-5 minutes apart.
The Hospitalist (a high risk OB), came in to see me. He had been consulting with MFM and with my OB. He told me they had decided together that it was not safe to send me home. They all agreed I should be admitted and that if the contractions wouldn't stop, they were going to take me in for a c-section that day. Either way, I was going to stay inpatient until delivery.
This was not the plan! I wanted to be home tucking Tayvri into bed that night. I wasn't ready. I had not packed or finished my to-do list!
I was supposed to have another week.
Trevor was amazing, reminding me that I had to take care of the baby inside of me now and that he and others would take care of everything else.
They moved me to my new room, N217. They bolused some IV fluids and administered nifedipine, which didn't seem to work so I then received a shot of terbutaline, and my first dose of steroids. The side effects of terbutaline were rough. I laid in bed feeling my heart pound in my ears and my whole body shake. I could hardly move around from all the monitors, IV lines, and SCD's. Trevor stayed by my side, afraid to leave. He slept in his clothes and contacts.My family brought Tayvri in to visit and she cried when I couldn't pick her up. Watching her leave felt like ripping a hole out of my chest.
The next day, my father came to administer with Trevor a priesthood blessing of comfort for me. In the blessing I again heard the words, "all is well", and was told to seek the scriptures for comfort. Trevor left for the first time shortly after that to go home and gather my things.
It was then, when I was alone for the first time in that room, that it felt so quiet..
I opened my scripture app on my phone and somehow it opened directly to this song; When Faith Endures:
Trevor would come join me for lunch. Then I would take an afternoon nap between visitors stopping by (so glad the post-co*id visitor restrictions had ended). They would do my second NST in the afternoon before shift change. In the evening, Trevor usually brought Tayvri to visit and we would have dinner together and then walk around the unit.
He would go put Tayvri to bed and come back to hang out with me late at night-I always felt like I was having my boyfriend over to my dorm room :). Trevor would snuggle into that small bed with me and rub my back and feet.
I would get my third NST right before bed. The nurses gathered vital signs every 4 hours during the day, but they mostly let me sleep uninterrupted.
I had a lot of things to help keep me busy, a roku, my laptop, books, scripture study material, self care items, and coloring supplies. Mostly I loved chatting and befriending the nurses. They probably don't know how much I valued their friendships there.
I also binge watched multiple seasons of SVU. I kept trying to tell myself to enjoy this "vacation" and rest before the baby came.
 |
| My typical breakfast. I always ordered a sugar free hot chocolate, it was my treat each day! |
 |
| My room was right next to a family room with a kitchenette. It had coloring supplies that Tayvri loved to use. |
The first week I was in relatively good spirits. Every time my contractions acted up, the medications were able to get them to subside. Tayvri went up north with my in-laws, which helped my mom guilt because I knew she was distractedly having fun.
The second week, I began having self-pitty parties. I missed my daughter. Everyday she would ask me if the doctor was going to take the baby out yet so that I could come home. It was heart wrenching every time I walked her out to the L&D doors to say goodbye.
Each night as Trevor left, my room would feel too quiet. That second week, I felt time was dragging by and started wishing they would just decide to do the c-section so that I could get on with my life.
Then a nurse reminded me that each day I put in antepartum, equaled to two less days of NICU time. That really put things back into perspective for me.
Though they had given me a tour of the NICU and talked me through what to expect, I dreaded seeing my tiny baby helpless in there. I knew I wanted to carry this baby as long as possible, as long as it was safe too.
So I decided to refresh my mindset. They had officially scheduled a c-section date for April 13, my 36-week mark. This was hopefully long enough for the baby to get the most benefit in the womb, but without putting the pregnancy at too much risk.
During my NST that evening, the baby had another variable. After a couple hours of extra monitoring, the Hospitalist cleared me once again. However, an hour after that, he came back to my room, finding Trevor snuggling with me in bed :) stating that my MFM had just called him. She was about to go to bed at home when she 'had a feeling' to check on my monitoring strips. When she saw that variable, it concerned her so she requested they keep me on monitors for most of the night and then start 4 x daily NST's tomorrow until delivery. So lucky me, I spent my birthday night on monitors.
The Delivery
The next day was Easter Sunday, I FaceTimed as Tayvri found her Easter basket. I started feeling sorry for myself again. It sucked missing the holiday morning with her. I pondered how next Easter will be so different with our family all together, including this new addition. Thankfully, Trevor brought Tayvri in to spend most of the day with me. I'm incredibly glad we had that day, because we had no idea it would be our last day as a family of 3!
After Trevor took Tayvri home, I started my third NST earlier than normal since we needed to do 4 now. On the NST they noticed I was having contractions which I had not been feeling while I had been busy with my daughter. It was a blessing in disguise that MFM had requested the extra NST.
They decided to keep me on the monitors again. After several bolus liters of IV fluids, and extra doses of nifedipine, my contractions were only becoming stronger and more regular. Over the two weeks I had been inpatient, this was probably the 4th or 5th time that I had been having steady contractions. However, this time was different because the interventions weren't slowing things down.Around 10pm the nurse came in and calmly told me that I should consider having Trevor come spend the night. It was the first time it hit me that I may be having a baby that day. The nurse explained that just in case delivery was imminent, it may be less likely for Trevor to miss it if he was already here.
Soon after Trevor arrived, an OB with my doctor's group came in to see us. She explained why they did not want to do more terbutaline; because if things turned into an emergency delivery, the cons outweighed the pro's.
My biggest fear was ending up in an emergency cesarean. I feared for the baby's life if a bleed began, and I was scared about the possibility of general anesthesia which would cause me to be asleep for the delivery.
I explained these fears to that OB. I would rather deliver now before it became an emergency. She concurred and left to quickly consult with the team.
She soon came back saying they all agreed that delivery now was the safest plan.
I remember my hands shaking and my heart racing as I signed consent forms. Suddenly my room was bustling with nurses and doctors. My contractions were now 2 minutes apart and getting pretty strong.
It was hard to believe that after all the months of living in constant fear from the VP, that within minutes from now, the baby would be here.
As they wheeled me to the OR, I tried to stay calm, taking deep breaths, reminding myself that millions of women before me have been wheeled into a sterile room just like this to have this same procedure done.
But I knew mine was going to be particularly complex. They would have to move fast. The baby's placenta was anterior, high enough to be out of the way itself, but the baby's blood vessels which crossed my cervix also crossed exactly over where the OB would need to cut.
The OB and I had discussed and prepared ahead of time for this. The plan was that once they cut through the sac and blood vessels, they would get the baby out within seconds and clamp its cord to stop further bleeding. They had blood products on hand for me and for the baby.

As I felt the spinal anesthetic spread through the lower half of my body, making me numb and heavy, I decided I wasn't afraid. I knew everything was going to be well.
I looked at Trevor as he held my face in his hands knowing we were about to meet our baby.
The whole OR crew was calming and the anesthesiologist (someone I knew from my nursing job) helped me try to relax and enjoy the moment.
Suddenly I heard the Doctor telling Trevor to stand up. The baby was already out. I could hear it's small squeaks. Trevor looked over the curtain and announced, "it's a Girl"!
What a shock! I truly thought it was a boy. Almost everyone thought it was a boy, including the Doctor.
Hot tears of joy soaked my eyes as they brought our little girl around to my face. So tiny, so precious. I wanted them to put her right onto my chest! However, they needed to assess her with the NICU team.
Trevor followed as they took her away. The rest of the c-section is a blur. As they wheeled me out to recovery, they stopped in the assessment room so that I could see our little girl. They held her at my side and told me she measured in at 5lb 5 oz and 18.5". That's when they told me she would need to go to the NICU for a while due to her breathing. I was sad to hear this, but grateful she was out safe.
I found myself in and out of sleep in the recovery room. An immense load felt lifted off my shoulders. My body had done it. It had carried this baby as long as It safely could. It was a hard, grueling and scary 8 months, but it was done now. She was here. I could hardly comprehend it.The OB would later tell me how miraculous my c-section was. Apparently I was having a silent placental abruption which was most likely the cause of the contractions. Also, he was millimeters away from cutting the largest baby blood vessel he had ever seen in a sac. It was a miracle he had missed it.
We were blessed that I had been in the hospital and being monitored closely. And we were right to make the decision to deliver that night. So many moments lined up, and I am convinced it was not all coincidence. I know there is a God, a loving Father who was orchestrating a safe arrival for this little girl.
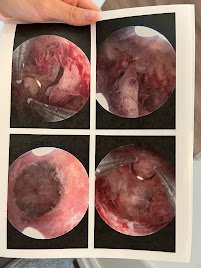
*If you enlarge the placenta images you will see the VCI (how the umbilical cord comes out of the sac and not the placenta at the bottom, notice the blood vessels spider through the sac). You can also see the large blood vessel that is roughly the diameter of a finger in the top left. You may need to google what a placenta should look like to compare the difference.*
The NICU
They transferred me to the postpartum unit. How strange it felt after 18 days in the same room to get a new room, with new staff that didn't know me. The most strange part though, was the feeling of missing a part of yourself.
For parents who have had infants in the NICU, I had never understood how difficult that is until experiencing it myself. To go from being pregnant with your baby as your constant companion, to being separated from them.. It was difficult. (So much love to all you NICU mama's, especially those who heart-wrenchingly will continue to be separated until you meet again in Heaven).
A little over 6 hours after delivery, I was finally ready to go see our baby girl again. They got me up into a wheelchair and took me down to the NICU.
What a strangely large room for such a small human.
She had a lot of cords and wires attached to her. It didn't look natural.
Thankfully she was breathing on her own, but her lungs were small and wet and not opening up well. So they had her on a pressurized (CPAP) nasal cannula. She also was on a glucose IV drip with the IV in her head, along with all the vital machine monitors.
We decided we would name her Mayla. A beautiful and sweet name for our feisty little Survivor.
Her middle name is Mari (pronounced Mar-ee). This is a combination of her grandmothers names, Cari and Margie, two incredible women who spent many hours in prayer for the arrival of this little miracle.
We surprised our family and loved ones with a texted picture of the baby. Everyone was expecting my delivery to be Thursday, and it was amusing to hear everyones reactions to the Monday morning surprise.
I had to go back upstairs for pain medications and breakfast. As delightful as it was to finally stuff my face with pancakes and syrup, a sense of yearning to be downstairs enveloped me. I didn't want our daughter to be alone in that huge room.
My mom came with Tayvri, who was ecstatic that the Doctor had finally taken the baby out so that I could come home. I had to break the unfortunate news to her that it would be a couple more days.
The NICU made an exception to their current rule (no visitors under 14) and allowed Tayvri in to meet Mayla.
I had dreamed of the moment my first triple rainbow baby would met this triple rainbow baby. Two living miracles that were created in a lab at the same time 5 years ago. Both our third rounds of implantation. It was surreal watching them meet.
Tayvri looked over all of Mayla's little features and declared that she loved her.
After Tayvri and grandma left, I was finally allowed the honor of holding Mayla. She felt so tiny! Tayvri had been 3lbs larger at birth and I was pretty sure I had never held such a small baby before. Though I know the NICU often see's baby's much smaller, I couldn't believe how little she seemed on my chest. And she had so much dark hair. She was beautiful.
After holding her for a couple hours, I needed pain medications and the bathroom. The nurses helped me stand up to transfer back to my wheelchair. As I stood, I felt the room spin and begin to turn black. I told the nurse I was going to faint.
That's how, 11 hours after I delivered Mayla, I passed out in the NICU.
I remember feeling stuck between a dream and reality, hearing voices calling my name but unable to respond.
The nurses called a “rapid response” on me. I woke up in a different room, on a stretcher, with a dozen nurses and doctors around me. How embarrassing I thought! Eventually they decided I was bleeding somewhere internally. (My H&H dropped to 17&5).
I remember waking up in that moment with an intense fear they would need to do an emergent hysterectomy.
So many thoughts went through my head. Would this be my last pregnancy? I’ve always known that it could be, but a hysterectomy would make that definitive.
What if I died.
Maybe this seems dramatic, but I had never faced the idea of my mortality in such a moment before.
I squeezed my husbands hand and prayed. I wanted to rest and enjoy the postpartum experience, even if it didn’t look the way I hoped.
I didn’t want the ending of this birth story to be a hysterectomy. And thankfully it wasn’t. They determined the bleeding had stopped on its own. Though I have been left with a large sub-dermal hematoma which is still slowly dissipating.
I did need two blood transfusions to get me back up and running. When the nurse came in to start my blood transfusion, I felt like crap. My lips were ghost white. My brain was foggy. Every time I turned my head, the whole world would spin. Apparently this is what it feels like to have critically low blood levels.
That’s when I noticed something was wrong with my husband. He was also ghost white and appeared nauseated. I asked him what was wrong and he admitted to me that he was dealing with a kidney stone.
Can you think of a worse timing?
I had never seen Trevor in so much pain before. And he was putting on a brave face as he knew I was going through so much at that moment. But I told him to go check into the ER and get himself taken care of.
So that’s how I found myself alone in my postpartum room, after a c-section, receiving a blood transfusion, while pumping milk for Mayla in the NICU.
I began to cry as I realized that 3 members of my family were in 3 separate hospital rooms at that moment.
I think that through the whirlwind of Mayla’s rapid delivery, I hadn’t let myself feel everything yet.
And everything felt out of my control.
I prayed aloud to my Heavenly Father for strength and healing over my family. I admitted that I couldn’t get through this alone and I needed help.
And strength beyond my own came.
With God's grace, we all made it through that night.
Over the next several days, as much as we hoped Mayla's lungs would rapidly improve, they didn't. And sorrowfully, I had to discharge and go home without her.
21 days inside the hospital, being high risk and watched over carefully, my every move monitored by nurses and doctors. And now they were allowing me to walk myself out the front door and leave. It felt unnatural!
I drove us home from the hospital at discharge because Trevor was on pain medications for the stone.
It was like déjà vu seeing the outside world and remembering what freedom felt like.
Except all I could really think about was how we were leaving Mayla there, alone in that big room. Although, she wasn't truly alone, because amazing nurses were with her. It still feels so wrong to go home without your baby.
We didn't stay home for long before we were back at the hospital. The next few days were a constant back and forth juggling our time between Tayvri and Mayla. That's when I asked Trevor to administer a Father's blessing to Mayla.
Immediately after the blessing, she started making quick progress towards going home! Over night she went from high flow oxygen needs to barely 0.01Lpm in her nasal cannula. She also excelled at breastfeeding and got the NG tube removed. The last step for her to go home was a room air trial and 24 hours of breastfeeding.
 |
| So happy to have the NG tube out! |
It was a rough night. There was no bed, only a flat couch that was shorter than me. My fresh abdominal incision made it very difficult to get up and down by myself. My legs were also thick as tree trunks, swollen with fluids and it was a real struggle!
I knew that if we made it through the night, we would get to go home.
I had never been so happy to see the sun come up!
Trevor came in and we sat there with Mayla while the NICU team completed one last rounding. 7 days on the inside and it was finally time to break out!
Here are some adorable photos of her on oxygen at home:
We are indeed grateful to finally have our family all under one roof. Now, 5 months later, it almost seems like a distant memory.
It has been surprisingly difficult to finally write this all down. There is a lot of trauma to unpack... but it is also filled with miracles and my testimony. So if you took the time to read this blog, which is really more of a journal entry, thank you.
It is my witness that Heavenly Father is aware of all the details. When I started my infertility journey 12 years ago, I never could have imagined the roads it would take me down. I am forever blessed to have my two earth-side daughters and my 6 angel baby's watching over us.
I am grateful to have the opportunity to share our story.
*Below are more of Mayla's newborn photos, done by Dayna Taylor Photography. It was beautiful to finally see her little face without any cords, tubes, or wires connected to her.*




























































































































































Comments
Post a Comment